Brucella IgG ELISA Kit
Regulatory status: For research use only, not for use in diagnostic procedures.
2. Sample Diluent: 1 bottle (ready to use) 22 ml
3. Calibrator: 1 Vial (ready to use) 1ml
4. Positive Control: 1 vial (ready to use) 1ml
5. Negative Control: 1 vial (ready to use) 1ml
6. Enzyme conjugate: 1 bottle (ready to use) 12ml
7. TMB Substrate: 1 bottle (ready to use) 12ml
8. Stop Solution: 1 bottle (ready to use) 12ml
9. Wash concentrate 20×: 1 bottle 25ml
2. Keep microwells sealed in a dry bag with desiccants.
3. The reagents are stable until expiration of the kit.
4. Do not expose test reagents to heat, sun or strong light.
This method uses B. abortus outer membrane, which is shared by the other species. Brucella IgG and IgA antibodies persist for many years after infection. A significant increase in Brucella IgG level is in patients with symptoms of brucellosis is indicative of recent exposure. IgM antibodies are present in acute brucellosis and also found in about 33% of patients with chronic brucellosis.
| Product Name | Cat. No. | Applications | Host Species | Datasheet | Price | Add to Basket |
|---|
| Product Name | Cat. No. | Applications | Host Species | Datasheet | Price | Add to Basket |
|---|
Brucellosis is a zoonosis with multiple clinical manifestations caused by Brucella infection. Brucella is a parthenogenetic intracellular parasite that efficiently colonizes cells of the macrophage lineage and replicates in large numbers in the liver and spleen after infection of humans. The bacterium not only has the ability to resist phagocytic bactericidal action, but also enables the host cell to form a microenvironment conducive to its survival and reproduction, and to survive for a long period of time within the host cell, culminating in a chronic persistent infection.
The prolonged presence of Brucella in host cells and its ability to escape immunity are the main reasons for the development of brucellosis as a chronic disease. Brucella interacts with lipid rafts on the surface of the cell membrane and enters the macrophage, forming Brucella-containing vesicles (BCV) surrounded by phagocytic vesicles. BCV interacts with early endosomes to acquire early markers, which allow the endosomes to mature in membrane-bound vesicles, forming acidified endosomes. At this point BCV is referred to as endosomal brucella⁃containing vacuole (eBCV). As BCV develops and matures, the Type Ⅳ secretory system (T4SS) mediates interactions between effector proteins and endoplasmic reticulum exit sites and acquires membranes of endoplasmic reticulum and Golgi origin. After the loss of early labeling molecules, eBCV gains lysosomes labeling molecules (e.g., Rab7, Lamp-1, etc.). BCVs that escape Lys degradation reach the ER and fuse with the ER in a SAR1- and RAB2-dependent manner, at which point the BCV is termed a repetitive vesicle-containing brucella⁃containing vacuole (rBCV). Later in the infection, rBCV transforms into a vesicle-containing autophagic brucella⁃containing vacuole (aBCV). aBCV does not continue to mature, and the organism ultimately releases the pathogen through lysogenic and nonlysogenic mechanisms, and the end of the intracellular cycle of brucellosis.
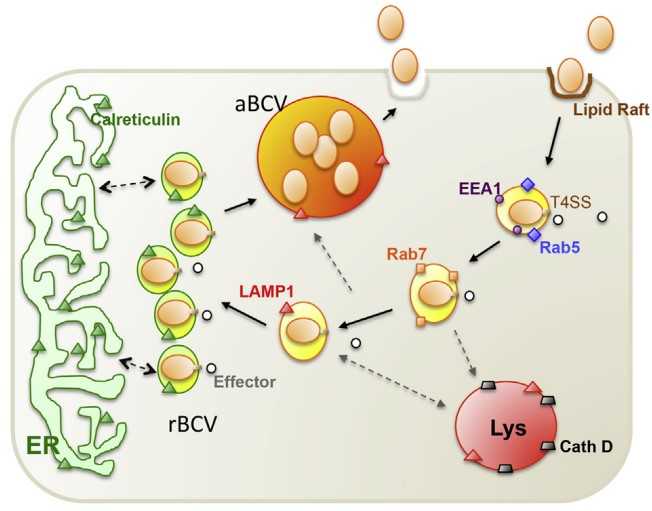 Figure 1. Working model of Brucella intracellular trafficking in macrophage cells
Figure 1. Working model of Brucella intracellular trafficking in macrophage cells
(Source: de Figueiredo P, et al. 2015)
Traditional laboratory tests for Brucella can be categorized into culture methods, identification methods, serologic methods, and nucleic acid assays. Isolated cultures of Brucella are usually considered the gold standard for the laboratory diagnosis of brucellosis. Patients with brucellosis experience bacteremia in the early stages of the disease, and performing blood cultures at this stage increases the rate of positive cultures. Serologic testing is by far the most commonly used method of confirming the diagnosis, and is usually employed as a screening test followed by more specific confirmatory tests on positive specimens. Nucleic acid testing is an emerging test for rapid and accurate diagnosis of brucellosis and typing of brucellosis, and a variety of molecular diagnostic techniques have been applied in the field of scientific research for the detection of brucellosis.
References
1. de Figueiredo P, et al. Pathogenesis and immunobiology of brucellosis: review of Brucella-host interactions. Am J Pathol. 2015 Jun;185(6):1505-17.
2. Głowacka P, et al. Brucella - Virulence Factors, Pathogenesis and Treatment. Pol J Microbiol. 2018 Jun 30;67(2):151-161.
Invoice / Purchase Order
Credit card
![]()