Glomerular mesangial cell recruitment and function require the co-receptor neuropilin-1
AMERICAN JOURNAL OF PHYSIOLOGY-RENAL PHYSIOLOGY
Authors: Bartlett, Christina S.; Scott, Rizaldy P.; Carota, Isabel Anna; Wnuk, Monika L.; Kanwar, Yashpal S.; Miner, Jeffrey H.; Quaggin, Susan E.
Abstract
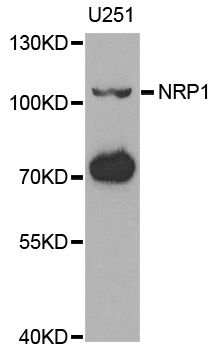
Proteinuria has been reported in cancer patients receiving agents that target the transmembrane receptor neuropilin-1 (Nrp1) suggesting potential adverse effects on glomerular function. Here we show that Nrp1 is highly expressed by mesangial cells and that genetic deletion of the Nrp1 gene from PDGF receptor-beta(+) mesangial cells results in proteinuric disease and glomerulosclerosis, leading to renal failure and death within 6 wk of age in mice. The major defect is a failure of mesangial cell migration that is required to establish the mature glomerular tuft. In vitro data show that the potent chemotactic effect of PDGFB is lost in Nrp1-deficient mesangial cells. Biochemical analyses reveal that Nrp1 is required for PDGFB-dependent phosphorylation of p130 Crk-associated substrate (p130Cas), a large-scaffold molecule that is involved in motility of other cell types. In stark contrast, matrix adhesion and activation of ERK and Akt, which mediate proliferation of mesangial cells in response to PDGFB, are unaffected by the absence of Nrp1. Taken together, these results identify a critical cell-autonomous role for Nrp1 in the migratory behavior of mesangial cells and may help explain the renal effects that occur in patients receiving Nrp1-inhibitory drugs.
Phase I study of capecitabine, oxaliplatin, bevacizumab, and everolimus in advanced solid tumors
INVESTIGATIONAL NEW DRUGS
Authors: Rangwala, Fatima; Bendell, Johanna C.; Kozloff, Mark F.; Arrowood, Christy C.; Dellinger, Andrew; Meadows, Jennifer; Tourt-Uhlig, Sandra; Murphy, Jennifer; Meadows, Kellen L.; Starr, Aijing; Broderick, Samuel; Brady, John C.; Cushman, Stephanie M.; Morse, Michael A.; Uronis, Hope E.; Hsu, S. David; Zafar, S. Yousuf; Wallace, James; Starodub, Alexander N.; Strickler, John H.; Pang, Herbert; Nixon, Andrew B.; Hurwitz, Herbert I.
Abstract
Purpose To define maximum tolerated dose (MTD), toxicities, and pharmacodynamics of capecitabine, oxaliplatin, bevacizumab, and everolimus in advanced solid tumor patients. Design This was a standard "3 + 3" dose-escalation trial. All subjects received bevacizumab 7.5 mg/kg on day 1 of each cycle. Doses for capecitabine, oxaliplatin and everolimus were modified per dose limiting toxicity (DLT). Baseline and on-treatment plasma biomarkers were analyzed. Archived tumor mRNA levels were evaluated for NRP1, NRP2 and VEGF-A isoforms. Results Twenty-nine patients were evaluable for toxicity and 30 for efficacy. Two DLTs were observed in cohort 1 and one DLT each was observed in cohort -1 and -1b. Grade a parts per thousand yen3 toxicities included neutropenia, hypertension, perforation/fistula/hemorrhage, hypertriglyceridemia, diarrhea, and thromboembolism. Twelve subjects experienced partial response (PR); 12 had stable disease as best response. Three of seven chemorefractory metastatic colorectal cancer (mCRC) subjects experienced PR; 8 of 15 chemonaive mCRC subjects experienced PR. Plasma T beta RIII and IL-6 increased on treatment but without correlation to outcome. Increased VEGF(165) levels significantly correlated with longer progression free survival. Conclusions Everolimus with full dose capecitabine, oxaliplatin, and bevacizumab had unacceptable toxicity. MTD was: everolimus 5 mg daily; capecitabine 680 mg/m(2) BID days 1-14; oxaliplatin 100 mg/m(2) and bevacizumab 7.5 mg/kg, day 1. Activity was noted in mCRC.
![]()