Type 2 diabetes mellitus (T2DM) is a metabolic disorder characterized by chronically elevated blood glucose levels. It typically results from inadequate insulin secretion because of dysfunction of the insulin-secreting pancreatic beta cells. At present, several oral antidiabetic medications are used for the treatment of T2DM including, α-glucosidases inhibitors, biguanides, sulfonylureas, meglitinides, GLP-1 receptor agonists (GLP-1RAs), peroxisome proliferator-activated receptor γ (PPAR-γ) agonists, dipeptidyl peptidase-4 (DPP-4) inhibitors, and sodium–glucose transporter 2 (SGLT2) inhibitors. In recent years, GLP-1RAs have become well-established therapies in T2DM.
The role of GLP-1/GLP-1R in human physiology
GLP-1, a product of the glucagon gene, is produced in L-cells of the small intestine. After food intake, the active form of GLP-1 is released into the circulation and activates specific G-protein coupled receptors. GLP-1R activation leads to a rapid increase in the levels of cyclic adenosine monophosphate (AMP) and intracellular calcium followed by glucose-dependent insulin release. The GLP-1 hormone is rapidly inactivated by the enzyme DPP-4, with a half-life of only 1–2 min. Amino acid modifications in the N-terminus and at certain positions in the C-terminus are involved in the resistance to DPP-4 inhibition, thus prolonging its half-life.
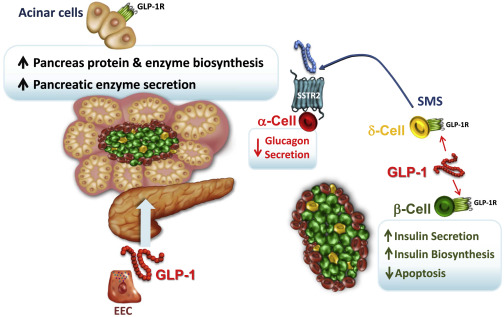 Fig. 1 Pancreatic Endocrine and Exocrine Actions of GLP-1 on Islet and Acinar Cells (Drucker DJ. Cell Metab. 2018)
Fig. 1 Pancreatic Endocrine and Exocrine Actions of GLP-1 on Islet and Acinar Cells (Drucker DJ. Cell Metab. 2018)
GLP-1/GLP-1RA and derived metabolites
The active form of GLP-1 is GLP-1(7–36) amide, which represents a major secretory product. However, the native GLP-1 peptide does not seem to be suitable for long-term treatment of patients with type 2 diabetes mellitus, primarily owing to its low stability in vivo.
GLP-1RA
GLP-1 therapies have been established using two main approaches: DPP4-resistant GLP-1 agonists/GLP-1RA and DPP-4 inhibitors, both of which aim to prolong the life-time of circulating GLP-1(7–36) amide. GLP-1RAs are useful tools for the treatment of T2DM, especially for patients aiming weight loss or to hypoglycaemia.
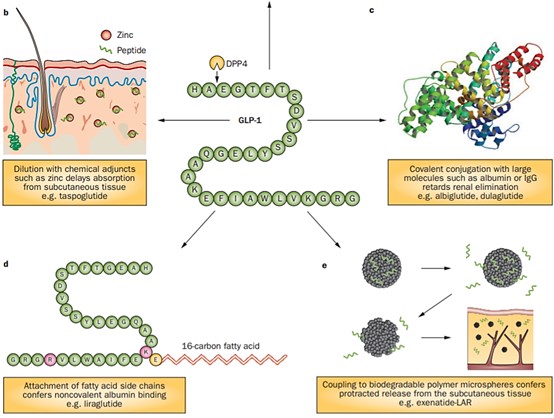 Fig. 2 Strategies employed to develop GLP-1 receptor agonists with prolonged in vivo half-lives. (Meier JJ. Nat Rev Endocrinol. 2012)
Fig. 2 Strategies employed to develop GLP-1 receptor agonists with prolonged in vivo half-lives. (Meier JJ. Nat Rev Endocrinol. 2012)
- Exenatide
Exenatide has 53% homology with GLP-1. It has a strong binding ability to GLP-1 receptor and is not easily degraded by DPP-4. Following peripheral administration, exenatide has been shown to suppress food intake via vagal-dependent and vagal-independent pathways that result in the direct activation of GLP-1R in the central nervous system.
Liraglutide is derived from human GLP-1-(7-37), and it has 97% amino acid homology to endogenous human GLP-1. With a fatty-acyl moiety on the GLP-1 peptide backbone, it has an increased half-life as a result of DPP-4 resistance and non-covalent binding to serum albumin.
- Albiglutide
Albiglutide is a long-acting GLP-1RA. Amino acids 1–30 and 31–60 constitute two copies of modified human GLP-1, the alanine at position 2 having been exchanged for a glycine for better DPP-4 resistance.
Semaglutide has 31 amino-acid containing peptidic structure which is 94% homologous to the native GLP-1 for avoiding immunogenicity. It is available as monotherapy in both subcutaneous as well as oral dosage form (first approved oral GLP-1 receptor agonist).
DPP-4 inhibitors
DPP-4 inhibitors have broad therapeutic applicability. To date, several small molecule DPP-4 inhibitors (vildagliptin, sitagliptin, saxagliptin, lina-gliptin, and alogliptin) have been used as treatments for type 2 diabetes to improve glucose tolerance. In addition, studies have shown that DDP-4 vaccines and inhibitory anti-DDP-4 antibody also have therapeutic potential due to their ability to improve glucose metabolism in mice.
Targets of other T2DM-related drugs
SGLTs
SGLTs are a family of transmembrane proteins that play a crucial role in the transport of glucose and sodium ions across cell membranes. T2DM patients have much higher SGLT2 expression in their kidneys than do healthy individuals. SGLT2 inhibitors act by blocking the action of the SGLT2 protein in the kidneys. This protein is responsible for reabsorbing glucose back into the bloodstream, but SGLT2 inhibitors prevent this from happening, resulting in increased glucose excretion in the urine, which improves glycemic control in people with T2DM.
PPAR-γ
PPAR controls the expression of a number of genes involved in adipocyte cell development and lipid and glucose metabolic pathways. PPAR-γ ligands may influence the activity of the renin–angiotensin system by transcriptional regulation at both the mediator and receptor levels, in addition to lowering blood glucose levels.
SUR 1
Sulfonylurea drugs affect sulfonylurea receptor 1 (SUR 1), which leads to the closure of adenosine triphosphate (ATP)-dependent potassium channels, preventing potassium from leaving the cell and depolarizing the cell membrane, leading to an influx of calcium and triggering insulin release.
References
- Drucker DJ. Mechanisms of Action and Therapeutic Application of Glucagon-like Peptide-1. Cell Metab. 2018 Apr 3;27(4):740-756.
- Sposito AC.; et al. GLP-1RAs in type 2 diabetes: mechanisms that underlie cardiovascular effects and overview of cardiovascular outcome data. Cardiovasc Diabetol. 2018 Dec 13;17(1):157.
- Youssef ME.; et al. Unlocking the Full Potential of SGLT2 Inhibitors: Expanding Applications beyond Glycemic Control. Int J Mol Sci. 2023 Mar 23;24(7):6039.
- Meier JJ. GLP-1 receptor agonists for individualized treatment of type 2 diabetes mellitus. Nat Rev Endocrinol. 2012 Dec;8(12):728-42.
- Pfeiffer AF, Klein HH. The treatment of type 2 diabetes. Dtsch Arztebl Int. 2014 Jan 31;111(5):69-81; quiz 82.
Creative Diagnostics offers a wide range of antibodies against GLP-1, GLP-1R, and DDP4, which are widely used in the study of drugs for type 2 diabetes. We also provide paired antibodies, the details are as follows.
DPP-4
DPP4 plays a major role in glucose metabolism. It is responsible for the degradation of incretins such as GLP-1.
| Target | Cat. No | Product Name | Application | Recommended antibody pair (Capture - Detection) | |
| DPP-4 | DCABY-4035 | Rat Anti-Human DPP4 (34-766) monoclonal antibody, clone 333224 | WB, FC, ELISA | DCABY-4035 - DPABY-473 | Inquiry |
| DPABY-473 | Goat Anti-Human DPP4 polyclonal antibody [Biotin] | ELISA | DCABY-4035 - DPABY-473 | Inquiry | |
| CABT-B1429 | Mouse Anti-Human DPP4 (Extracellular) monoclonal antibody, clone 0G2.3 | WB | Inquiry | ||
| DCABH-432 | Mouse Anti-Human (full length) DPP4 monoclonal antibody, clone 22E8 | WB, IHC-P, FC, ICC/IF | Inquiry | ||
| DCABH-2135 | Rabbit Anti-DPP4 monoclonal antibody, clone KN22-53 | WB, ICC/IF, IHC, FC | Inquiry | ||
| DPAB-DC777 | Mouse anti-Human DPP4 (352-451) polyclonal antibody | WB, ELISA | Inquiry | ||
| DPABH-02444 | Rabbit anti-Human DPP4 (internal region) polyclonal antibody | IHC-P | Inquiry |
GLP-1
Glucagon-like peptide-1 (GLP-1) is a peptide hormone deriving from the tissue-specific posttranslational processing of the proglucagon peptide. It has the ability to decrease blood sugar levels in a glucose-dependent manner by enhancing the secretion of insulin.
GLP-1RA
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of drugs that reduce blood sugar and energy intake by activating the GLP-1 receptor. They mimic the actions of the endogenous incretin hormone GLP-1 that is released by the gut after eating.
| Target | Cat. No | Product Name | Application | |
| Liraglutide | CABT-Z391R | Rabbit anti-Liraglutide polyclonal antibody | ELISA | Inquiry |
| Semaglutide | CABT-L6359 | Rabbit Anti-Semaglutide polyclonal antibody | ELISA, IA | Inquiry |
GLP-1R
The glucagon-like peptide-1 receptor (GLP1R) is a G protein-coupled receptor (GPCR) found on beta cells of the pancreas and on neurons of the brain. It is involved in the control of blood sugar level by enhancing insulin secretion.
| Target | Cat. No | Product Name | Application | |
| Human GLP-1R | DCABH-5062 | Mouse Anti-Human GLP1R monoclonal antibody, clone 2I5 | IHC-P | Inquiry |
| DCABH-15518 | Rabbit Anti-Human GLP1R monoclonal antibody | WB, ELISA | Inquiry | |
| DMAB-JXL23100 | Mouse Anti-Human GLP1R (24-145) monoclonal antibody, clone 4G63 | ELISA, BL, IF, IHC, WB | Inquiry | |
| DPAB-JXL23238 | Rabbit Anti-Human GLP1R (24-175) polyclonal antibody | WB, IHC-P, IF | Inquiry | |
| Mouse GLP-1R | DMAB-JXL23101 | Mouse Anti-Mouse GLP1R (full-length) monoclonal antibody, clone 8G49 | ELISA, FACS, IF, IHC, WB | Inquiry |
| Rat GLP1R | DPAB-JXL23239 | Rabbit Anti-Rat GLP1R (101-200) polyclonal antibody | WB, ELISA | Inquiry |